Videos
September 20, 2023 | By Admin
Shimspine Chronology and Analysis Consulting
October 6, 2021 | By Dr. Shim
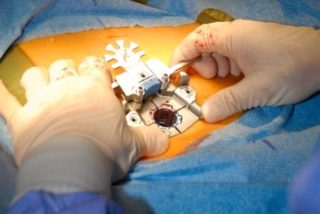
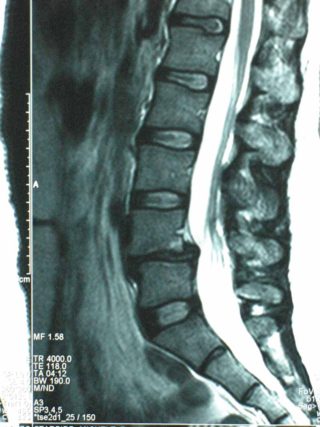
Is Percutaneous Discectomy Better Than Traditional Discectomy?
October 1, 2021 | By Dr. Shim
Artificial Cervical Disc Replacement
August 12, 2021 | By Dr. Shim
Spine Injuries in Baseball
August 5, 2021 | By Dr. Shim
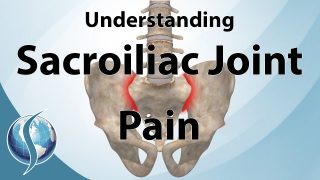
Does Spinal Manipulative Therapy Work for Lower Back Pain?
Expert Opinions, Evaluations, and Education.
ABOUT ShimSpine
Why ShimSpine?
Dr. Shim is an Orthopaedic Spine Surgeon and leading Medical Expert in the Tampa Bay area since 1993.
Learn More