Neck Pain
Neck Pain
Most commonly, neck pain presents with gradual stiffness, and areas of tenderness to the upper back, and trapezius muscles. Often times, there is no history of a significant trauma or injury. Something as innocent as a cough, sneeze, or a startling reaction can set the neck pain in motion. The typical patient will describe having a bit of stiffness and soreness. After a night of sleep, there is increasing stiffness and pain with movement of the neck. Usually, it localizes to an area of the neck. Occasionally, there is radiating sensations to the arms and hands.
As a clinician, initial neck pain evaluation should be done to rule out a potential serious condition. The major concerns would be a fracture, infection, or a tumor. Any history of a traumatic injury, fevers, unintended weight loss, and night sweats should increase the index of suspicion. A thorough physical exam is necessary to make sure there is no evidence of point bony tenderness, areas of warm and redness, bruising, or significant neurologic deficit. If any of these findings are present, further diagnostic testing and specialist referral is prudent.
If these signs are not present, most likely, the patient is experiencing the effects of a strain to the many neck muscles, or manifestations of degenerative disk disease. In other words, the wear and tear of activities of daily living. In patients without any suspicion for fracture, tumor, infection or neurologic deficit, the best options usually are the judicious use of medications, and some stretching exercises. Typically, most patients with neck pain will resolve or diminish their symptoms within 4-6 weeks.
But of course, most people find it difficult to be patient while in neck pain. In this world of instant gratification, there is a rush to do x-rays, MRI’s and advanced therapies. But as long as the patient does not have any indication for the above serious problems, they will most likely get better with time. As physicians, we will get credit for initiating care, medications, tests, etc. if patients get better. But in reality, most people will get better no matter what. That is why we often find ourselves explaining to painfree patients about their degenerative findings (degenerative disk disease) on an X-ray or MRI. We caution them on the natural wear and tear process and the likelihood of recurrence of pain. Enough studies have shown the only way for patients to minimize recurrence of these pains is to participate in a regular stretching and exercise program.
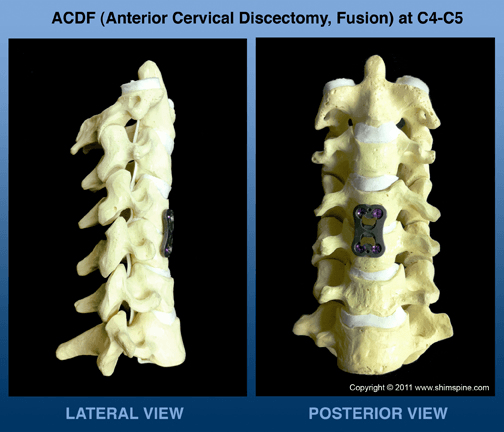
After 6 weeks, however, if there is persistent pain, then a referral for further studies, or evaluation by a specialist would be reasonable. In regards for the need for neck surgery, it is usually for patients with a well defined problem that does not improve. It usually means the patient has severe unremitting pain, progressive neurologic deficit, or a worsening infection or tumor. The true chance of the need for cervical surgery is less than a few percent of patients who present with neck pain. Occasionally, however, the patient will need the picture below:
Last modified: October 22, 2019