Anomalies That Can Affect Your Neck Surgery
What are the test results that may matter for surgeries in your neck?
Not everyone is born with the standard bones of the spine.
In fact, a significant portion of the population has what is called an anatomic variant.
But there’s no need to be alarmed.
Having an anatomic variant simply means that a structure deviates from the most common form found in the species. Note that we don’t use the term abnormality because of the negative implication.
So where does this anatomic variant become an issue? For spine surgeons, a test is performed before surgery to identify such variants. The surgeon may need to make accommodations if the tests come back positive. It certainly can be a source of added precaution because of the potential complications if they are not considered.
In this video, we’ll discuss the more common variants found in the neck. If you read these findings on your CT, MRI or X-ray report, you might be confused and want to know what they mean.
Let’s start with KFS, Klippel-feil syndrome. What is it?

Klippel-feil syndrome syndrome occurs when two or more vertebrae are fused together from birth. While this congenital fusion may be picked up on X-rays, sometimes it’s not that obvious. Some variations of KFS are so subtle that doctors mistake the two fused bones for one. This mis-count can then lead to surgery on the wrong levels of the neck.
While KFS has been associated with a short neck, and reduced neck motion, there are plenty of people who remain unaffected by it. In the latter case, KFS is identified incidentally after obtaining an X-ray.
Upon discovering this variant, the surgeon may need to adjust their surgical approach. What confuses people are the inconsistencies due to the highly variable nature of KFS. If you see this finding on your report, it’s worth discussing the ramifications with your surgeon.
Before we dive into the next variant, a little anatomy lesson is in order.
There are blood vessels that go into the back of the brain called the vertebral arteries. Like the name suggests, they are paired arteries that travel through the neck, and help form the circle of blood vessels that supply the brain.
The path of the vertebral artery is important for those with the findings of an arcuate foramen, also known as ponticulus posticus which is Latin for “little posterior bridge”. Interestingly, various studies show that up to 15% of the population has some form of arcuate foramen.
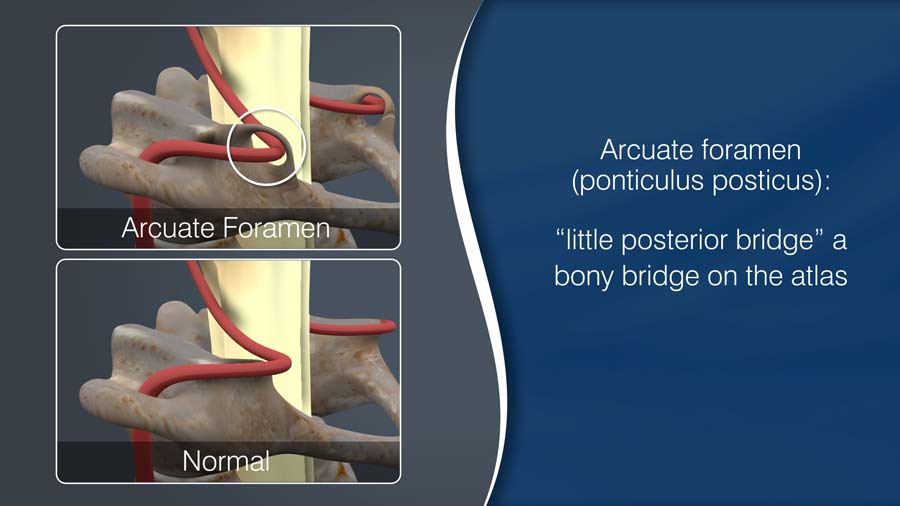
For a person with this variant, the path of the vertebral artery might deviate from the norm. Precautions should be taken when operating on the relevant parts of the cervical spine. Doing so will reduce the risk of injury to the blood vessel during dissection. Because the artery may be encased in bone, standard approaches to the bones and joints of the upper neck may not be possible without damaging the artery.
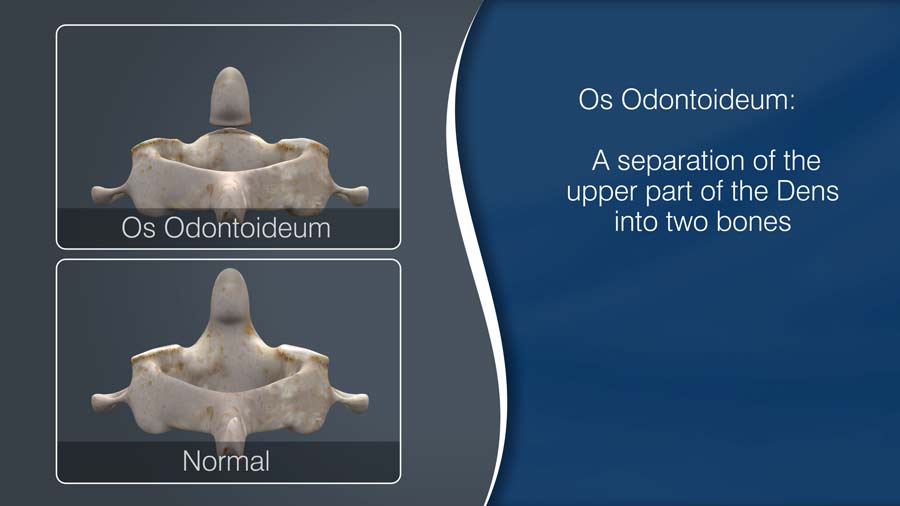
The next variant I’ll be discussing is the Os Odontoideum — a separation of the upper part of the Dens into two bones.
But first, let’s go over some anatomy so you can make sense of what this means.
Your head essentially swivels around your neck. The upper most bone of the neck is a ring structure named the Atlas, also known as the C1 bone. This bone rotates around a post, which is called the Axis, also known as the C2 bone. The Dens is the actual projection off the main body of the C2. As you can see, this relatively simple arrangement allows your head to rotate around your neck. This C1-C2 configuration is responsible for up to 50% of your total ability to rotate your head.
In the Os Odontoideum variant, the Dens is what is separated.
An Os Odontoideum can be caused by trauma, present from birth, or even naturally develop over time.
Like KFS, Os Odontoideum is often discovered incidentally.
For some, however, it can be associated with various symptoms, such as neck pain, headaches, and unusual nerve complaints like shooting pains to the arms with motion, or tingling to the back of the head to the upper neck.
Upon discovering this variant, the spine specialist must be vigilant and do their best to prevent this from becoming something more serious.
Additional testing, such as flexion and extension X-rays, are necessary to see if there is an associated instability with this variant. If there is, there will likely be a comprehensive evaluation to discuss the pros and cons of undergoing surgery. Most instabilities require surgical intervention.
Now, for our last variant: what is an anomaly of the foramen transversarium?
Again, let’s first look at the anatomy.
The Foramen transversarium are paired holes in the cervical bones, by which the vertebral arteries travel from the lower neck to the brain.

It turns out that the configuration of these holes, and their relationship to the vertebral arteries do not always follow a standard pattern.
Certain surgeries require dissection and removal of disc and bone material from the front of the neck bones. During these dissections, the Surgeon might discover that the holes and the location of these blood vessels are not in their typical place.
Surgeons usually use high speed burs and electrocautery during neck spinal surgeries. These tools should be avoided on the vertebral arteries — so if an anomaly of the foramen transversarium is found, the surgeon should use that information to minimize the risk of injury to these blood vessels during dissection.
When preparing for neck surgeries, testing should identify klippel-feil syndrome, uncommon blood vessel locations, and the presence of an os odontoideum.
If you do see these findings in your test results, understand they can be incidental and not the source of your complaints.
And if you are scheduled for surgery, a specific variant may be the reason your surgeon chooses a particular operation for your condition. Most surgeons will not mind discussing these findings with you.
Let me reassure you. There is no need to be alarmed if you happen to have an anatomic variant. Share your concerns with your surgeon but rest assured that they have likely already planned around them.
Thanks for reading.
Citations
- Hedequist DJ, Mo AZ. Os Odontoideum in Children. J Am Acad Orthop Surg. 2019 Aug 5; PubMed PMID: 31393315
- Tins BJ, Balain B. Incidence of numerical variants and transitional lumbosacral vertebrae on whole-spine MRI. Insights Imaging. 2016 Apr;7(2):199-203. PubMed PMID: 26873359
- Young JP, Young PH, Ackermann MJ, Anderson PA, Riew KD. The ponticulus posticus: implications for screw insertion into the first cervical lateral mass. J Bone Joint Surg Am. 2005 Nov;87(11):2495-8. PubMed PMID: 16264126
- Zibis A, Mitrousias V, Galanakis N, Chalampalaki N, Arvanitis D, Karantanas A. Variations of transverse foramina in cervical vertebrae: what happens to the vertebral artery? Eur Spine J. 2018 Jun;27(6):1278-1285. PubMed PMID: 29455293
Last modified: October 28, 2020









