Does Discectomy Lead to Spinal Fusion?
If you have had a lumbar disc surgery, does that mean you will have a fusion surgery in the future?
This is a very common question asked by many. If you have a back operation, does not mean you will have more in the future?
More specifically, if you have a lower back discectomy surgery, does that mean you will have a more significant fusion operation in the future?
As a spinal surgeon, I know that is a possibility. But how frequently does it really happen?
This is the best way I can answer this question. Do you have more than a 50% chance of having a fusion operation after you have had a lumbar discectomy? The answer is a definitive no.
Before we get into the specifics, we do need to make sure everybody understands the difference between these two operative procedures.
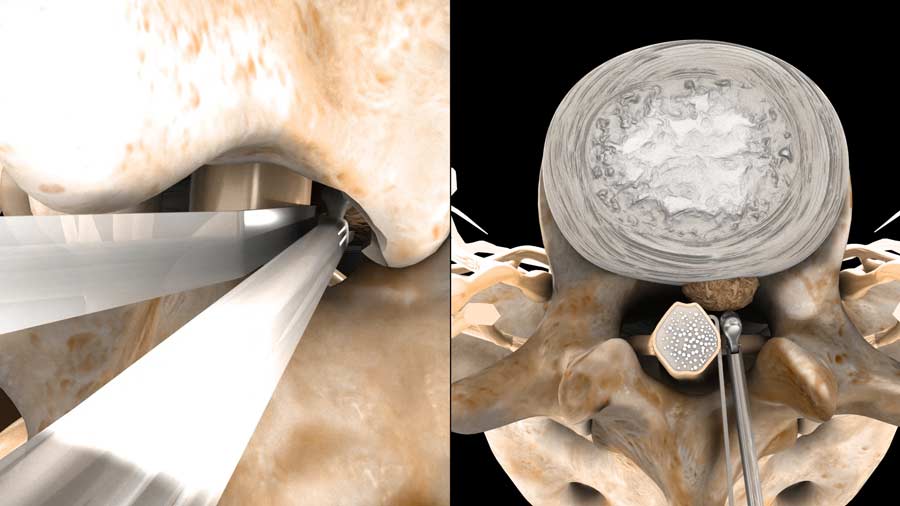
Discectomy means removing a piece of disc from the back, that is a source of pain. Most the time, the reason you would have this surgery is because the disc component is pressing on a nerve and causing a very defined pain, numbness, and weakness pattern. Statistically, properly chosen patients who undergo discectomy surgery have about a 95% chance of success after the operation. Success being defined as a significant decrease in pain and the ability to return back to normal functions. Please note, there may still be some residual numbness and some pain, but the person is able to get back to activities. Currently there is about 450,000 lumbar discectomies being performed in the United States on an annual basis.

A fusion surgery is different. Fusion means making the body think 2 separate bones are actually a broken bone, and the body then mends the 2 broken bones together. The reason fusions to the lower back are performed is because abnormal movements between the bones cause intermittent or constant irritations of the nerves near these bones. The medical term is instability. Instability can be caused by a congenital problem, degeneration, and even more serious conditions like broken bones, cancer, or infections. Fusions are much bigger operations, and unfortunately not as predictable in their ability to return patients back to full activity compared to a discectomy. Latest information indicates approximately 200,000 elective lumbar fusion operations being performed in the United States annually.
If you just take the raw numbers, you can mistakenly think that anybody with a discectomy will have a moderate chance that they will have a fusion operation at a later time. But the numbers are misleading, because many of the lumbar fusion operations are also been performed for diagnoses such as scoliosis, spondylolisthesis, spinal stenosis, and more serious conditions including cancer and infection.
In March 2019, a paper was published by Castillo, et al from the University of Chicago Medical Center.
While it was a retrospective review, it followed approximately 200,000 discectomy patients, to identify the rate these patients will have lumbar fusions, compared to a matched group of patients with similar diagnoses who did not have any operation at all.
While the patient’s with discectomy did have a higher rate of fusions overall, the actual percentage of patients with prior discectomies who ended up having fusions after 10 years was less than 9%.
The author compared their data to other reports. Depending on the country of origin, the fusion rates could be significantly lower. A study from Finland had around 5%. There has been other studies following discectomy with fusion rates significantly less than 5%.
The bottom line is the rate of fusion surgery after discectomy is not very high.
Another factor that must be considered is the changing number of fusions that are being performed in the United States compared to the past.

From 2004, to 2015, there has been a 62% increase in the use of fusions In the USA. While there has been some aging of the population, we cannot explain the significant increase in the use of this technique solely by clinical outcomes.
There has been enough studies to show that despite increasing utilization of advanced spine technologies and spinal operations, it has not resulted in any better clinical outcomes, return to work, return to function, or improved healthcare parameters.
Costs have significantly gone up. Various entities have generated significant revenue from this trend.
But, the health of the population did not improve. It is no wonder the payors of these expensive treatments are questioning their efficacy and justification.
Sorry to digress, and lets get back to the main point of the video.
To summarize, while discectomy is a beneficial surgical treatment for the right patient, the concerns for needing a future spinal fusion should be taken into the context of the statistics.
From a large population standpoint, the chances of needing fusion surgery after a lumbar discectomy is less than 10% over 10 years, in the United States. It is even less in other first world industrial nations.
The rates of additional fusion has also been my experience. The vast majority of my patients did well after discectomy, especially at the L5-S1 levels.
Fusions in my practice were limited to patients who had instability secondary to spondylolisthesis, multiple recurrent disc herniations, or in the more serious conditions of infection, fracture, or tumor.
If you are having discectomy surgery, while there is potential for a fusion at a later time, the risks are relatively small. But please have that discussion with your surgeon.
If you would like more information about similar topics, Please subscribe to our newsletter or our YouTube channel.
Citations
- Castillo H, Chintapalli RTV, Boyajian HH, Cruz SA, Morgan VK, Shi LL, Lee MJ. Lumbar discectomy is associated with higher rates of lumbar fusion. Spine J. 2019 Mar;19(3):487-492. PubMed PMID: 29792995
- Martin BI, Mirza SK, Spina N, Spiker WR, Lawrence B, Brodke DS. Trends in Lumbar Fusion Procedure Rates and Associated Hospital Costs for Degenerative Spinal Diseases in the United States, 2004 to 2015. Spine (Phila Pa 1976). 2019 Mar 1;44(5):369-376. PubMed PMID: 30074971
Last modified: July 17, 2020










My surgeon is recommending decompression at T12 and a fusion at L2 to treat an extruded herniated disk. I am almost completely pain free. I had a lot of weakness in my thighs but I’ve had significant improvement over the last 2 weeks. This is my first herniation. Would a micro discectomy be a better option?
My husband has been diagnosed with a herniated disc and severe spinal stenosis.The orthopedic surgeon tells us to have a discectomy and the neurologist says to have a TLIF ..why two different opinions?!!
You will have to ask the surgeons. There are various options to each condition. Some surgeons will do the least invasive first. Others will recommend the most invasive. There has to be a reason for both.
I had a disectomy on my L4 -L5 it herniated in the same spot 10 months later but this time worse . Would u recommend a disectomy again or a fusion being it failed already
In general, fusion should be avoided if possible. If the reason you have another disc herniation is secondary to instability, fusion may be a better option. Please discuss with your surgeon.
That is a very individual circumstance. Sometimes, it will be better to do the least invasive option. Other times, if there is instability, or the need of a significant bone removal to remove the new herniated disc, a fusion may be a reasonable option. Please discuss with your surgeon.
I have had discectomies at L5-S1 and later L4-L5.
The first was in 2012 and the latter was in 2019. My issue is that the numbness subsided, but the pain is much greater now. Mornings, I can barely sit up and put my shorts on because I can’t bend. This will be forward, but it hurts to even arch my back to clean myself after going to the bathroom. I cant lean over on my counter without my back locking up and being in excruciating pain.
My question is should I ask my neurologist about a fusion and do you believe it would help with the pain?
Thanks,
Tony Webb
Surgery is always the last choice. Make sure to explore options including therapy, exercise, weight loss, etc. Fusions work, but not as predictably as other surgeries.