Posterior Cervical Foraminotomy
Here’s what you need to know about posterior cervical foraminotomy:
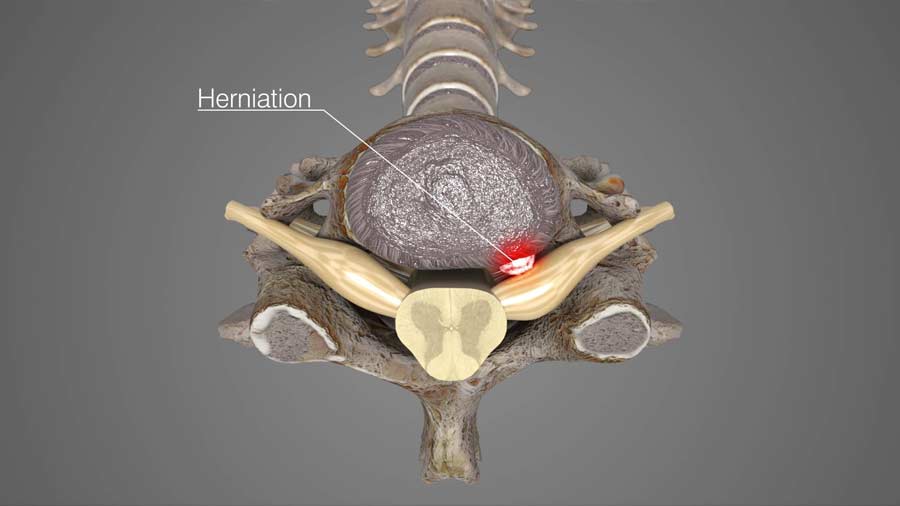
The purpose of posterior cervical foraminotomy is to alleviate the spinal nerve compression caused by a specific type of disc herniation or bone spur.
The surgeon makes a small incision on the back of the neck over the intended surgical site. Various tissues and muscles are gently divided and retracted so the bone and ligaments covering the spinal cord are visible.

The nerve roots and other structures are carefully set aside so the surgeon is able to visualize and remove the offending material. Remember, posterior cervical foraminotomy works when the disc herniation or bone spurs are located towards the side of the spine, and away from the centrally located spinal cord. If the disc herniation is located in the center, there is concern about moving the spinal cord to reach the herniation or bone spur. Too much pressure on the spinal cord can cause damage. The surgeon must select the right situation to offer this operation.
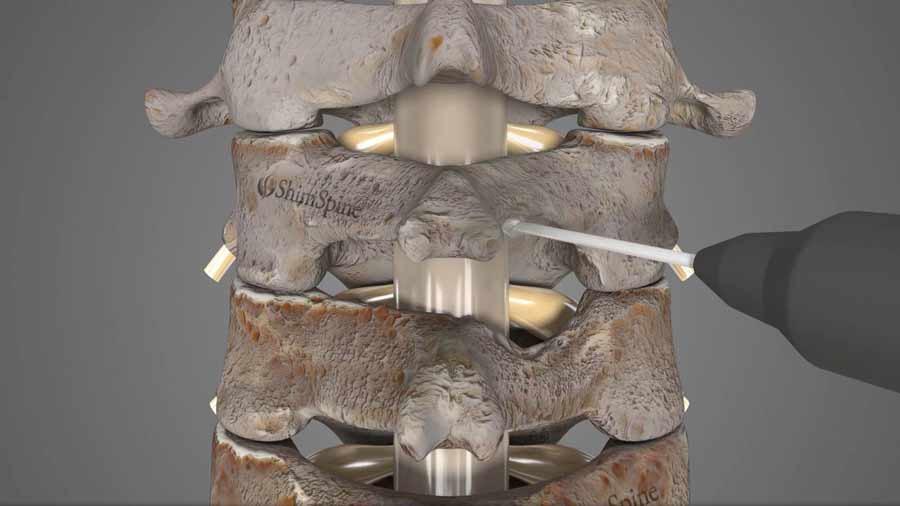
Both the bony overgrown and a portion of the lamina bone are removed using tools such as burs, kerrison rongeurs, and curettes. By providing more space for the nerves, the surgeon reduces the pressure and alleviates the associated pain.
Fluids are used to wash away any bony debris from the mechanical tools used for dissection. The layers that were divided are then sutured back up and the incision is closed with surgical glue.
The minimally invasive surgery is relatively quick with an average surgery time of two hours, although this does vary depending on the number of spinal levels involved.
Why get it?
Your surgeon has considered this surgery if the examinations they conducted are consistent with your symptoms of pain, and the cause of the pressure on the nerve can be removed without excessive retraction of the spinal cord.
The immediate success rates reported by patients after receiving posterior cervical foraminotomy are extremely high. Long term success rates are more variable but still range from 75 to 90%.
The standard surgical options for neck decompression are posterior cervical foraminotomy and anterior cervical discectomy and fusion. I talk about ACDF procedure in my last video — please click on the link below if you’d like to watch it. Generally, the decision to choose between these two alternatives are based on the location of the nerve compression, and the nature of the pain. Please discuss your options with your surgeon.
What are the Potential complications?
Well, the excellent success rate of posterior cervical foraminotomy is primarily due to the careful selection of patients. Most symptoms caused by a pinched nerve, and they do get better with nonsurgical treatment over time. Surgery should only be considered after all nonsurgical options have been exhausted.
Some patients have shown to suffer from same-segment and adjacent-segment disease following the operation. A study analyzed the outcomes of 303 patients and found there was a 3 to 5% risk of developing this adjacent level disease. In some cases, this requires patients to undergo additional operations. Greater neck pain prior to the surgery correlated to higher rates of reoperation. Any questions or specific concerns, again should be discussed with your doctor.
What are the recent trends?
The transitions from traditional or “open” posterior cervical foraminotomy to minimally invasive posterior cervical foraminotomy shows how much surgical techniques have improved over the years. Although there haven’t been many studies directly comparing the two methods, one does show that the minimally invasive approach tends to result in a faster recovery. Minimizing the risk and optimizing patient outcomes have become easier with the availability of minimally invasive exposure techniques.
I hope this blog/video helped broaden your understanding of posterior cervical foraminotomy. Until next time, this is Dr. John Shim.
Additional References:
https://thejns.org/spine/view/journals/j-neurosurg-spine/10/4/article-p343.xml
Citations
- Bydon M, Mathios D, Macki M, de la Garza-Ramos R, Sciubba DM, Witham TF, Wolinsky JP, Gokaslan ZL, Bydon A. Long-term patient outcomes after posterior cervical foraminotomy: an analysis of 151 cases. J Neurosurg Spine. 2014 Nov;21(5):727-31. PubMed PMID: 25127430
- Platt A, Gerard CS, O'Toole JE. Comparison of outcomes following minimally invasive and open posterior cervical foraminotomy: description of minimally invasive technique and review of literature. J Spine Surg. 2020 Mar;6(1):243-251. PubMed PMID: 32309662
- Clarke MJ, Ecker RD, Krauss WE, McClelland RL, Dekutoski MB. Same-segment and adjacent-segment disease following posterior cervical foraminotomy. J Neurosurg Spine. 2007 Jan;6(1):5-9. PubMed PMID: 17233284
Last modified: March 3, 2021