The Right Words Matter
Do all Doctors use the same terms when describing Spine Disc findings on MRI’s?
Many of you have had MRI studies of your spine and had discussion with your Doctors about the findings.
Often times, it seems the doctors are using the terms disc bulge, or disc herniations interchangeably. It can get confusing. Both for the patient, and unfortunately, also the medical doctors who need to discuss the findings.
So, in order to come to some agreement on these terms, Doctors representing Spinal specialists and Radiologists formed a group to define these terms.
The last recognized effort resulted in the Publishing of an Article Called the Lumbar disc nomenclature: version 2.0 Published in the Spine Journal in 2014 by Dr. David Fardon.
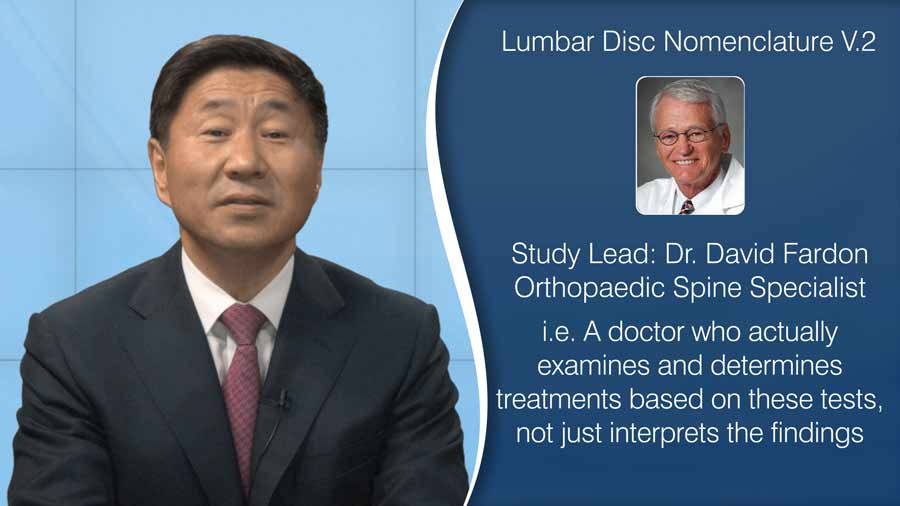
Very few know that this often referred article about standards of Reading MRI’s was Lead Authored by an Orthopaedic Spine Specialist, Dr. David Fardon. As a spine specialist, a Doctor who actually examines and determines treatments based on these tests, not just interprets the findings, he led this effort and publication.
This 2014 paper established a common naming protocol about Disc findings.
The authors took great pains to state that MRI findings by themselves cannot offer any information on whether the findings are caused by trauma, or a natural occurrence.
To directly quote the paper:
“The definitions of diagnoses are not intended to imply external etiologic events such as trauma, they do not imply relationship to symptoms, and they do not define or imply the need for specific treatment.”
To summarize the paper, Disc findings can be broken down to two main types.
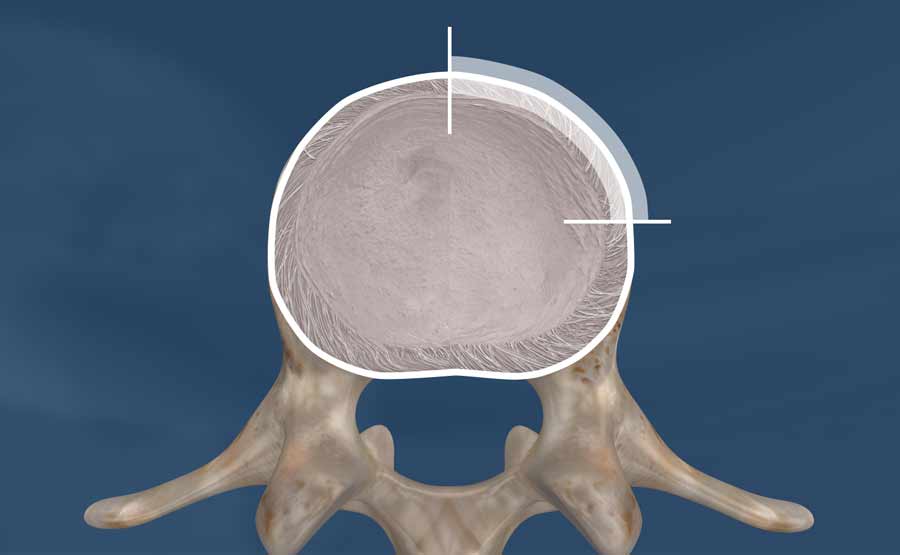
The first is a disc bulge, which is a uniform presence of disc material outside the walls of the spine bone. The paper used the term ring apophyses, but for the public, it is the margin of the spine bones. If you have seen our prior video about disc bulges versus herniations, it is the bulging of the tire wall concept. In certain deformities, such as scoliosis, there can be some asymmetry of the bulging, but it is still a bulge.
The second is the herniated Disc, where a focal or localized displacement of disc material occurs. My prior video explains this as the jelly donut model. Focal or localized is defined by displacement that is less than 25% of the circumference of the whole disc.
I have had many spirited debates on whether I should call herniations, protrusions or vice versa. Here is the direct quote on page 2,533 from this often referenced study:
“By exclusion of other terms, and by reasons of simplicity and common usage, ‘herniated disc’ is the best general term to denote displacement of disc material.”
Disc herniations can then be broken down into three different types.
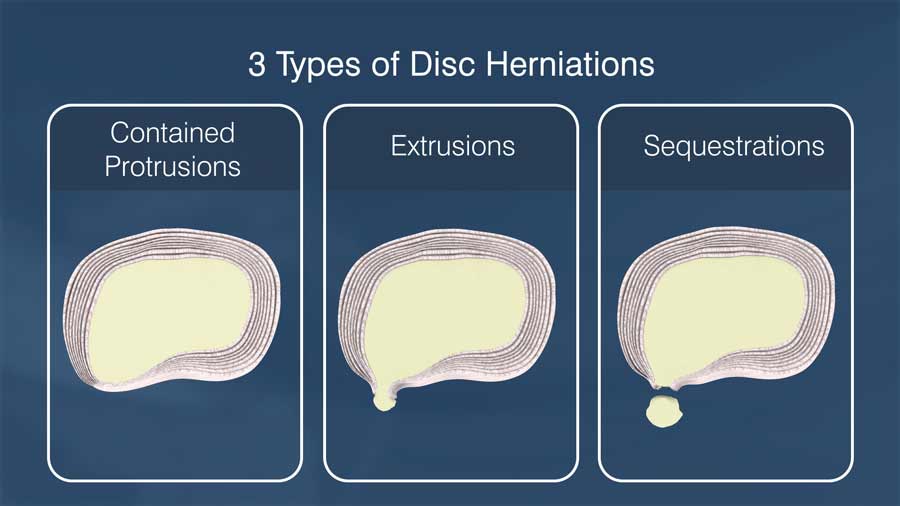
- Contained Protrusions, which are herniations that are still connected by intact outer fibers of the annulus.
- Extrusions which mean the disc herniation is no longer contained by the last fibers of the annulus.
- Sequestrations, which means the disc herniation is no longer in contact with the rest of the disc, and its own island of disc material.
In addition to the discussion about Disc Herniations and bulges, this paper establishes that breaks in the outside part of the disc called the annulus should be called fissures instead of tears. The term tear suggests a traumatic event, and it is well know that these annular disruptions can be a natural process not associated with any specific trauma. Since 1993, it has been established that having disc annular fissures, herniations, and degeneration is an expect part of life, and often times, these findings are not causing any pain to the person with these findings.
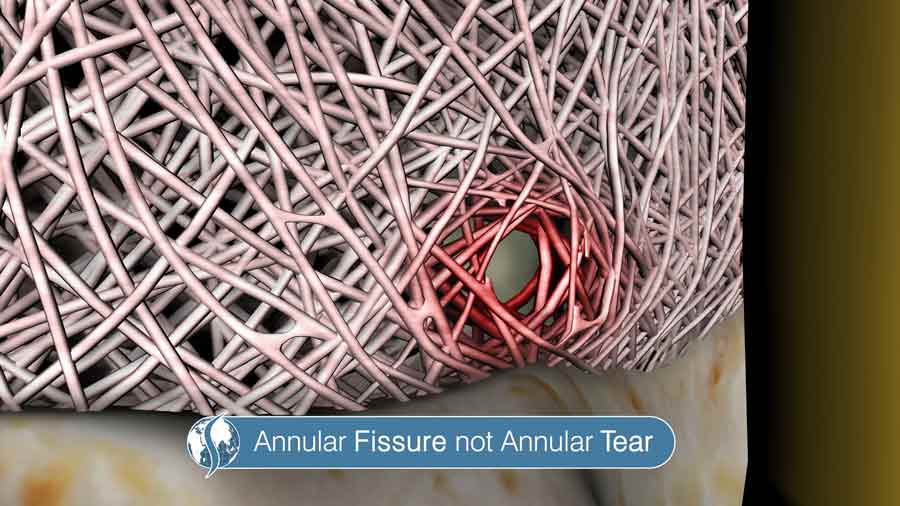
The paper also mentions various research studies that show almost every disc that degenerates or ages will have an annular fissure. It is a normal part of life like wrinkles, and thinning hair.
The final point of the paper is to discuss the so called High intensity zone. In the early 1990’s, these findings of an area of brightness on the annulus was thought to be a sign of an acute problem, and an indication of the cause of the pain. In the early 1990’s, many spine fusions were performed because of this finding on MRI, with unpredictable clinical results.
It turns out these High intensity zones represent fluid or granulation tissue in the annulus. The presence of the high intensity zone is not specific to a traumatic event, and is not always associated with any pain complaints. It may not even correspond to an annular fissure. Even today, its significance is not established, and debated.
To me, many parts of the Disc Nomenclature Study are consistent with what I already use in my practice. I define a bulge or a herniation. If asked to further clarify on the herniation, it is contained, extruded, or sequestered.
To me, the MRI by itself cannot be used to age when the disc finding was created.
To me, the presence or absence of a HIZ, has very little benefit in determining the treatment options for the patient. I learned from the 1990’s experience.
I have had the honor of listening to Dr. Fardon speak in past meetings. While he retired from practice a few years ago, he has left an impact on Physician Education, and will always be honored as one of the Greatest Teachers and Proponents of Rational, compassionate and competent Orthopaedic and Spine Care.
I hope you found this discussion interesting. Thanks for watching.
If you would like more information about similar topics, please subscribe to our newsletter or our YouTube channel.
Last modified: June 8, 2020









