What is a Nonunion?
What is a nonunion? For most doctors, it means two or more bones that were supposed to heal together but did not. To give an example, sometimes broken leg bones do not heal. Surgery may be necessary to unite the bone edges together. Nonunions can happen to any bone, although for most healthy people, the body usually can mend the broken bones without surgery.
For people who have certain spinal conditions, a spine fusion operation may have been performed. Usually the fusion is recommended because your Surgeon thinks you have an unstable spine, or to correct a spine curvature problem.
While spinal fusion surgery has its risks, in the United States, it is a common procedure. In this discussion, I will not discuss the risks or benefits of spinal fusion. Instead, let’s focus on what is a nonunion for a spinal fusion.
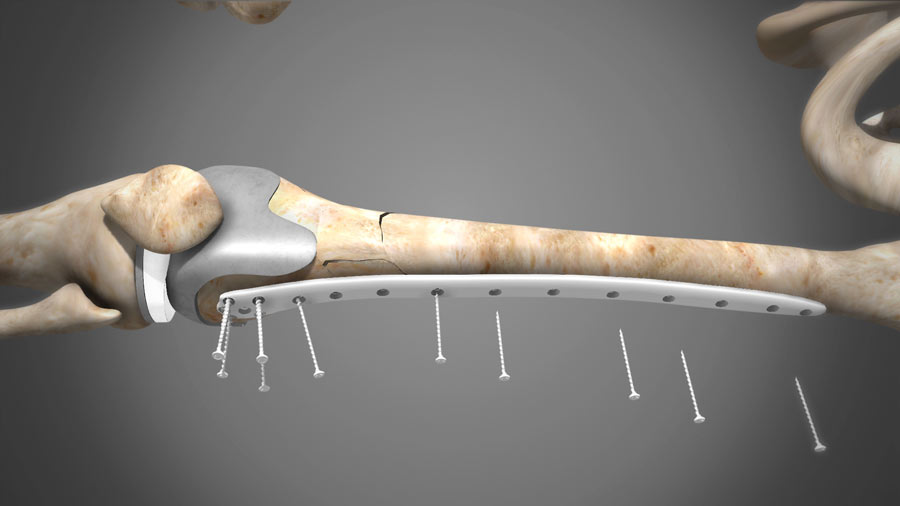
Contemporary spine fusion techniques utilize mechanical plates, screws, and or rods to hold the bones in place. Sometimes, it includes a cage device to provide added stability and a surface to promote fusion. The body mobilizes the specific bone-forming cells to create a boney bridge to unite the two or more bones. To promote healing, the bone surfaces are scratched to cause some bleeding. This effectively creates a similar situation as a broken bone. The body reacts by trying to heal this break.
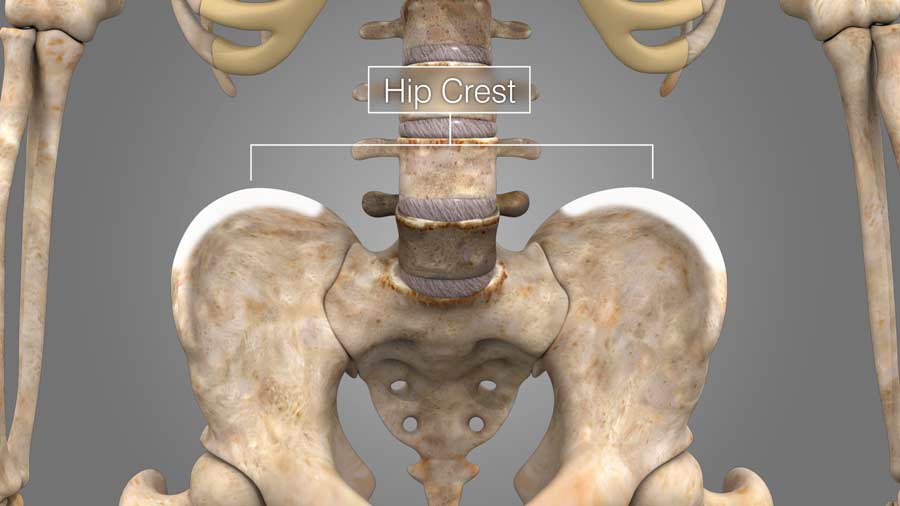
To aide in the fusion or uniting of the bones, bone tissue is obtained from your hip crest. This material is like a putty that helps unite the broken bones.
The hope is that the bones heal together, over time, thus achieving a fusion.
Unfortunately, the nonunion rates of fusion can be significant for certain situations.
Medical Risk factors for nonunion include smoking history, diabetes, osteoporosis, and steroid use.
Surgical factors include multiple levels of fusion, posterior only approach, and lumbar location.
Nonunion is associated with poorer outcomes and more pain after surgery.
So how do we determine if there is a nonunion? The most obvious sign is gaps without healing on x-rays. If there are concerns for nonunion, x-rays obtained when flexing and extending your spine can also demonstrate nonunion. Unfortunately, because the motion can be painful, a person may not give full flexion and extension effort. These x-ray views may not always show a nonunion. Right now, most will use thin cut CT scans to diagnosis a nonunion. Because most fusions now utilize plates, screws and or rods, another clue is the so-called halos around the hardware. Halos are caused by compressing the bones around the metal, because the motions are caused by a lack of union. Sometimes there are even broken screws or rods that should cause suspicion of a nonunion. (animate a broken rod, and show motion and halo of a screw while the spine flexes and extends).
So what should you do if you have a nonunion? That depends. Sometimes, the best option is to do nothing if you are feeling fine.
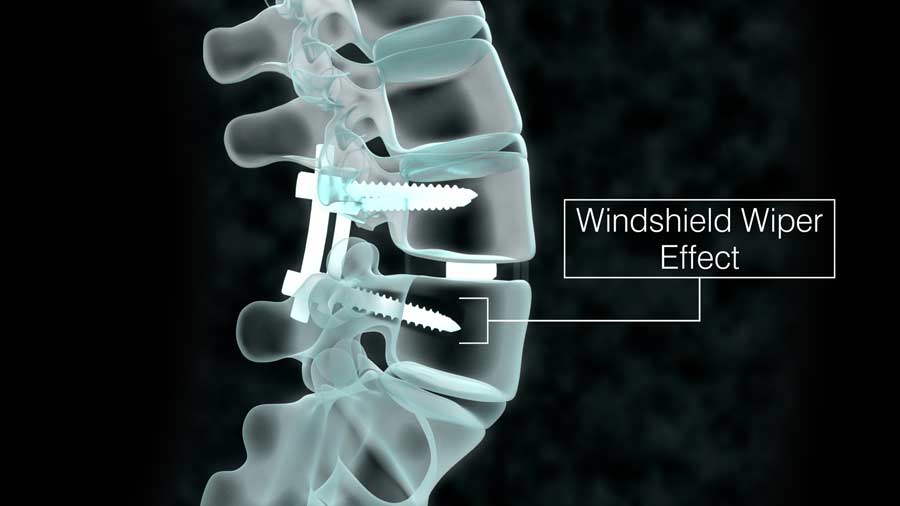
In other circumstances, the lack of fusion causes the metallic screws and rods to dig into the bones, causing the so-called windshield wiper effect. Because this puts important structures such as nerves or blood vessels at risk, the hardware should be removed, and if necessary another fusion attempted.
It is a potentially difficult decision for both the surgeon and the patient. IF you have these concerns, make sure to obtain a few opinions.
If you are contemplating a fusion operation, please be aware of this potential complication. Your surgeon will do their best to create the best fusion environment for your spine. Still, it is a possibility and if you have the risk factors mentioned above, please weigh them before deciding to have a fusion operation.
Additional Reference: How Many Spinal Fusions are Performed Each Year in the United States?
Last modified: November 18, 2020










My son is 15 and has a non union l5 pars defect. He is a wrestler and was diagnosed around 12/1/21. We started PT about 3 weeks ago, he’s feeling good. Whats going to be his limitations moving forward or will it eventually create a union?
I can only give general comments and cannot provide advise to any one person. In general, a spondylolysis (par defect) can get better with PT, and at times bracing. If the defect remains symptomatic (painful) or gets activated by activities, modifications to activities (rest) may be necessary for a certain period of time. IF the pain worsens, surgery can be an option. Please discuss your son’s situation with your doctor.
Hi Doctor ur videos r very informative and I do respect a lot. Sir I do have a query if you can respond Please, I had L5-S1 fusion due to bilateral pars fracture. I m concerned about adjescent disk diseases. I like to ask about how to minimize this risk in future for me and what are the option for artificial disk replacement and facet replacement T shim spine. I am from India and not lot of option available for this query here. I did lot of search and found GERMANY spine specialist do lot of such surgeries…need help doctor please reply
I hope the fusion helped. It is a good option for pars fracture with constant pain. There will always be risk of adjacent disc disease, but more surgery is not the solution. Keep your weight down. Low impact exercise, do not smoke, and avoiding heavy manual labor is the goal. It may not be obtainable for some, but those are factors anyone can directly control.